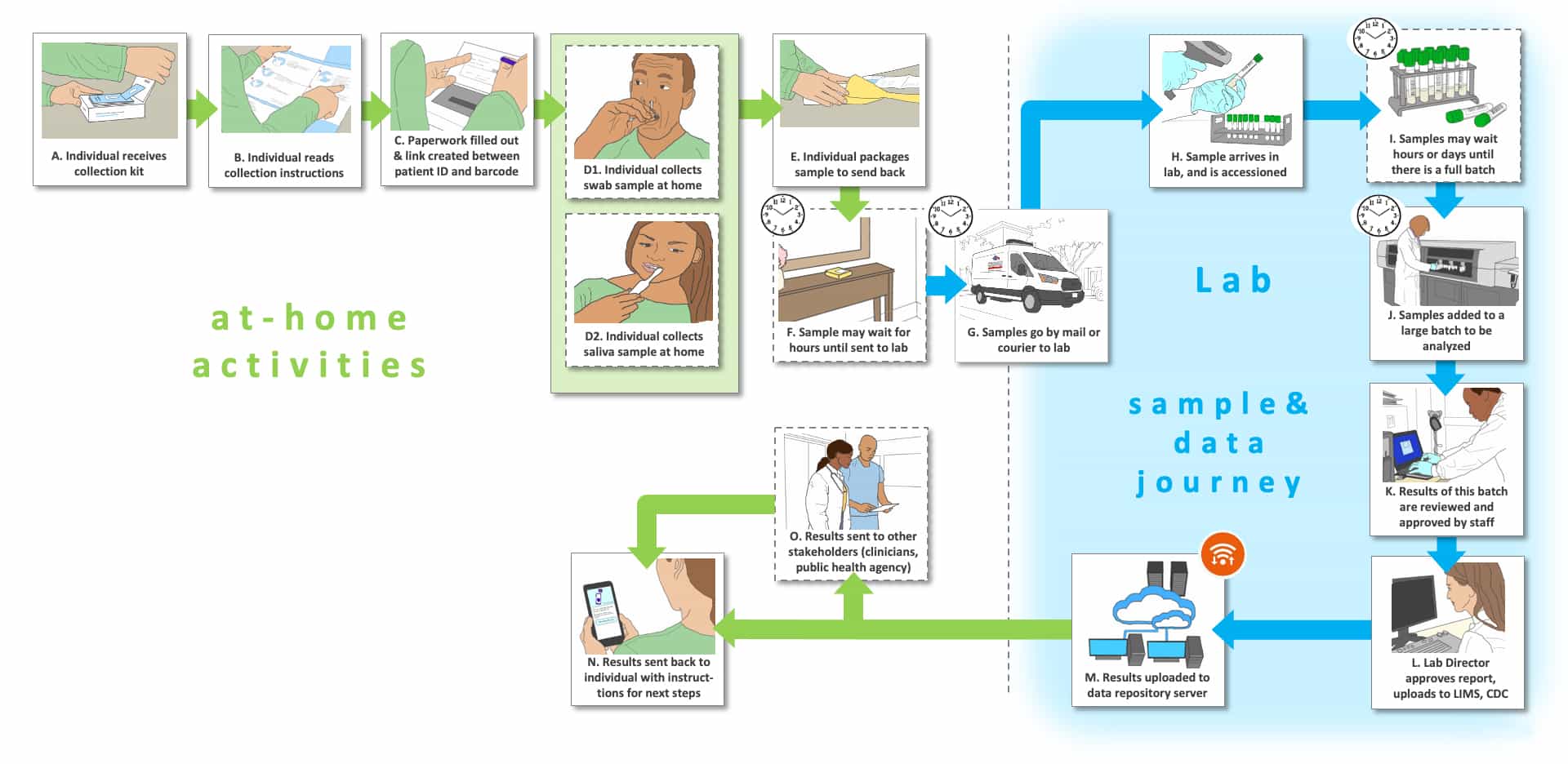
Storyboard I is based upon the use of samples collected at home instead of by a healthcare professional. Upon collection, the samples are packaged and delivered for shipment and off-site testing. This use setting is pertinent to several of the Use Cases (see Table 1; Use Cases 5-8, 10). The tests used can be RNA, antibody or antigen based.
Steps A-D are unique to this Storyboard series. Panel A depicts the opening of a sample collection kit, which is much like kits that might be provided for colorectal cancer screening or HIV self-tests. In Step B, the person to be tested reads carefully the instructions for use (IFU), then in Step C the person fills out paperwork and initiates the bar-coding process. At this point in Step D the individual collects the sample (e.g., simple nasal swab (D1) or saliva (D2)). The sample must be properly packaged (Step E) and sent by mail, picked up by a courier or placed in a collection box for pick up for delivery to the site of testing (Step G). The package could sit for some time before shipment, depending upon the schedule of the person to be tested (Step F). Upon shipment to the laboratory in Step G, the sample has entered the “sample and data” journey, while the patient stays home in isolation if needed (for the Use Cases diagnosis or differential diagnosis in a symptomatic individual) or continues with their typical daily activities (for Use Cases related to previous exposure determination, surveillance, or screening of non-symptomatic persons).
Upon receipt of the samples in the laboratory (Step G), samples are accessioned (Step H) and added to a batch of tests that will be tested. For some of the Use Cases (previous exposure, surveillance) the turnaround time is not a significant issue, so the size of the batch of tests could be quite large to keep the costs low, which could require a few days of deliveries before a large enough batch is assembled (Step I). For other Use Cases (diagnosis, differential diagnosis, screening), time-to-result could be critical so that the batch size might need to be smaller, but still cost-effective for the lab. Tests are performed, reviewed, recorded and the results are delivered (Steps J-M) to the person tested (previous exposure, surveillance) or to the healthcare provider and then to the person tested (diagnosis, screening), depending upon the Use Case (Steps N-O). Next steps could include self-isolation and/or seeking of care (diagnosis, screening). Alternatively, results could provide information concerning the likelihood of a previous infection (previous exposure, surveillance).
The major issue in home sample collection is that it must be conducted reproducibly and accurately by the person to be tested. Although self-collection would typically be performed alone at home while following written and/or pictorial IFU, there are organizations that use an on-line tutorial or live visual interactions with an instructor. The types of samples that can be collected at home are more limited than for lab testing. Home collection of nasopharyngeal swabs, bronchial lavage, and venipuncture blood are unlikely, while nasal, mid-turbinate, oropharyngeal swabs, finger prick blood and saliva samples can be self-collected, as demonstrated by a number of studies. EUA for collection of saliva samples has been issued for specific tests and collection devices.
Self-collection for shipment can dramatically improve the processing of people in need of testing by eliminating the need for long lines at sites of presentation. People that might not be willing to go to a site of sample collection can easily collect and send samples to testing labs without significant concerns of exposure to themselves or others. In some locations, anyone wishing to be tested can gain access to sample collection kits and the address of testing labs, however in other locations testing can only be initiated with a doctor’s prescription. Third party payment versus self-payment is variable and is usually dependent upon the policies of the lab associated with the collection kits and their association with payers.
In addition to at home self-collection, there is a trend toward the use of self-collection in a professional setting. The advantages are twofold. When the person to be tested spits into a tube or swabs their own nose they will not be exposing a healthcare professional to significant contamination, in contrast to when the sample must be obtained by direct interactions between the healthcare professional and the tested individual (e.g., nasopharyngeal swabs, venipuncture blood). Second, if there are a series of people waiting to be tested, one healthcare worker can provide collection kits to several people simultaneously who can collect their own samples in parallel. This in contrast to situations when a healthcare professional must collect samples in series one person at a time, which takes far longer to achieve the same goal.
Self-testing is the next time-saving step, whichis under development, after the implementation of the self-collection of samples. Antibody and antigen assays for self-testing have appeared (although with variable performance) and others will be introduced in the near future. The minimum test performance characteristics remain to be established. New Use Cases will need to be developed for these types of testing scenarios.
The Storyboards are meant to be approximate descriptions of the overall testing ecosystem. They are organized as flow charts containing sites of activity, people involved (e.g., patients, medical practitioners and laboratorians) and pathways for tested individuals, healthcare professionals (or other testers in some cases), sample collection and transport, testing, result generation and information flow. They also show key decisions informed by the test results.
There are three types of “journeys” in the Storyboards: 1) the tested individual’s (usually patient) journey which are shown using green arrows, 2) point-of-care or point-of-use activities which are shown with purple arrows (e.g., sample collection, sometimes testing) and 3) the sample and data journey through a laboratory, which is shown with blue arrows.
The letters that label each step are not meant to indicate an order for the steps, they are simply there to facilitate discussion about the storyboard. Optional steps have a dashed outline, and examples of possible variations in a step are labeled with the same letter followed by differentiating numbers e.g., B1, B2 and B3)
There are a number of clocks and calendars pictured near specific steps to indicate time-consuming steps and those that could vary in total time depending upon the workflow efficiency of the healthcare site and the characteristics of the testing platform (e.g., batch analysis, time to results).